
"Creating Awareness One Parish at a Time"
We are the VOICE and the STRENGTH for those who struggle for a diagnosis of dysautonomia, due to lack of education and awareness. We are the HELPING HANDS that find resources for our members and their caretakers, so no one travels this journey alone. We are here to bring KNOWLEDGE and AWARENESS to medical providers and the general public, so dysautonomia is no longer unheard of.
LET'S BE SOCIAL!

We aim to share our stories with hospitals, health care offices, families, and friends. Our goal is to find caregivers and individuals who go undiagnosed or misdiagnosed. We are here to inspire, advocate, be the example, pave the way, and cast a light into the vast darkness that comes with a chronic illness like dysautonomia. If we reach just one person, so they do not struggle for years to receive a diagnosis and proper treatment, then we have achieved our goal. We will work tirelessly until every parish, hospital, school, and community in Louisiana have been touched by our group.
DYSAUTONOMIA
[ dis-aw-tuh-noh-mee-uh ]
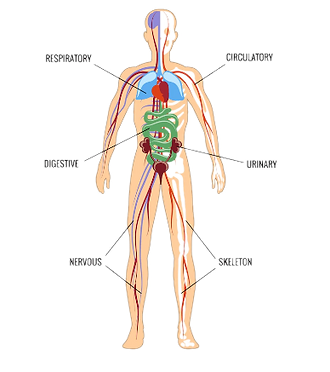
Dysautonomia, or autonomic dysfunction, is a condition which affects the proper function of the autonomic nervous system (ANS). This affects the heart, bladder, intestines, sweat glands, pupils and blood vessels.
-Cleveland Clinic
"Creating Awareness One Parish at a Time"

What is
DYSAUTONOMIA?
[ dis-aw-tuh-noh-mee-uh ]
"If you think dysautonomia is hard to say, try living with it..."
-Carmen Gonzales

Dysautonomia:
-
Refers to a group of medical conditions caused by problems with the autonomic nervous system (ANS)
-
Is also called autonomic dysfunction or autonomic neuropathy
-
Can occur as its own disorder, without the presence of other diseases. This is called, primary dysautonomia. In many cases, treatment of primary dysautonomia is symptomatic and supportive
-
It can also occur as a condition of another disease. This is called secondary dysautonomia. Secondary forms may improve with treatment of the underlying condition
-
Anyone can develop dysautonomia at almost any age. You may be born with a dysautonomia condition, or you may develop it gradually or quite suddenly at any age

Pictured above: The medulla oblongata location in the brain
The medulla oblongata is the bottom-most part of your brain where your brain and spinal cord connect, making it a key conduit for nerve signals to and from your brain and bodily systems.
It's the part of the brain that controls your involuntary bodily functions like your heartbeat, breathing, and digestion.
When the ANS doesn’t work as it should, something goes wrong in that bodily system.
There is NO CURE for dysautonomia, but there are ways to help alleviate or avoid symptoms.
-
Dizziness/Lightheadedness
-
Swings in Blood Pressure
-
Swings in Heart Rate
-
Heart Palpitations
-
Brain Fog
-
Fast/Slow Heart Rate
-
Migraines
-
Gastrointestinal Issues
-
Exercise Intolerance
- Heat/Cold Intolerance
-
Orthostatic Intolerance
-
Shortness of Breath
-
Fatigue

The symptoms can come and go, making them difficult to predict. Symptoms are different among people, which makes it hard to diagnose and treat.
There are various types of dysautonomia, each of which has different symptoms.
TYPES OF DYSAUTONOMIA
Dysautonomia is a medical term for a group of different conditions that share a common problem – improper functioning of the autonomic nervous system. Here are some of the conditions caused by primary dysautonomia.
NEUROCARDIOGENIC SYNCOPE (NCS)
1
POSTURAL ORTHOSTATIC TACHYCARDIA SYNDROME (POTS)
2
FAMILIAL DYSAUTONOMIA (FD)
3
MULTIPLE SYSTEM ATROPHY (MSA)
4
PURE AUTONOMIC FAILURE
5
Neurocardiogenic syncope (NCS): NCS is the most common form of dysautonomia. It can cause fainting spells that happen once or twice in your lifetime or multiple times every day. NCS is also called situational syncope or vasovagal syncope.
Postural orthostatic tachycardia syndrome (POTS): A disorder that causes problems with circulation (blood flow), POTS can cause your heart to beat too fast when you stand up. It can lead to fainting, chest pain and shortness of breath.
Familial dysautonomia (FD): People inherit this type of dysautonomia from their genetic relatives. It can cause decreased pain sensitivity, lack of eye tears and trouble regulating body temperature. FD is more likely to affect Jewish people (Ashkenazi Jewish heritage) of Eastern European heritage.
Multiple system atrophy (MSA): A life-threatening form of dysautonomia, multiple system atrophy develops in people over 40 years old. It can lead to heart rate issues, low blood pressure, erectile dysfunction and loss of bladder control.
Pure autonomic failure: People with this form of dysautonomia experience a fall in blood pressure upon standing and have symptoms including dizziness, fainting, visual problems, chest pain, and tiredness. Symptoms are sometimes relieved by lying down or sitting.
GETTING A DIAGNOSIS
Neurological Exam
If you have symptoms of autonomic failure, but no risk factors, the diagnosis can be more involved. Your health care provider will probably review your medical history, discuss your symptoms and do a physical exam, as well as blood work, to rule out other diseases or conditions.

*To find a local doctor to get a diagnosis,
please visit our Resources page or click here.
Autonomic Testing
These tests measure how your heart rate and blood pressure respond during exercises such as deep breathing and forcefully breathing out (Valsalva maneuver).
-
Quantitative sudomotor axon reflex test. This test checks how the nerves that manage your sweat glands respond to stimulation. A small electrical current passes through capsules placed on your forearm, upper and lower leg, and foot. A computer analyzes the response of your nerves and sweat glands. You might feel warmth or a tingling sensation during the test.
-
Thermoregulatory sweat test. You're coated with a powder that changes color when you sweat. While you lie in a chamber with a slowly increasing temperature, digital photos document the results as you begin to sweat. Your sweat pattern might help confirm a diagnosis of autonomic neuropathy or suggest other causes for decreased or increased sweating.

Tilt Table
test
This test monitors the response of blood pressure and heart rate to changes in posture and position. It simulates what occurs when you stand up after lying down. You lie flat on a table, which is then tilted to raise the upper part of your body. Typically, blood vessels narrow and heart rate increases to compensate for the drop in blood pressure. This response may be slowed if you have autonomic neuropathy.
A simpler test for this response involves checking your blood pressure when lying, sitting and standing after three minutes. Another test involves standing for a minute, then squatting for a minute and then standing again while blood pressure and heart rate are monitored.

TREATMENTS
Managing symptoms of a dysautonomia condition may require a multi-tiered strategy.
For example, you may need medications to restore autonomic function, but this may need to be supplemented with lifestyle changes that include diet, exercise and symptom-specific activities. This might include drinking more fluids and ingesting salt if you have blood pressure or heart rate issues, or adopting posture changes to help support blood circulation if fainting is an issue.
The central nervous system consists of the brain, spinal cord, and all of the nerves within our body. The autonomic nervous system is the part of the central nervous system that regulates involuntary body functions. Within the autonomic nervous system, we find the sympathetic and parasympathetic nervous systems, which both control the same parts of the body and same general functions of the body, but with opposing effects.


The body has become accustomed to such an ongoing cycle of intense stress, that it does not shift back unconsciously to the parasympathetic nervous system. A person suffering with chronic stress is in a constant state of fight-or-flight mode, where some or all of their autonomic functions are shut down, eventually leading to or triggering the many painful and debilitating aforementioned issues with the body. All of these symptoms, that are the actual function of the sympathetic nervous system, can eventually be prevented if one can shift out of sympathetic overdrive into parasympathetic and eventually reset autonomic balance (or homeostasis) and experience normal functions again.
Observe your own body too. Pay close attention to what seems to ease your symptoms or make them worse. Use a notebook or calendar to record trends and other insights that might help you manage your symptoms. Share your notes with your doctor so your healthcare team can better understand how your condition affects you.
DISEASES THAT CAUSE SECONDARY DYSAUTONOMIA
Autonomic nervous system disorders can occur alone or as the result of another disease, such as diabetes, Parkinson's disease, or alcoholism. Some types are temporary, but may worsen over time. Some autonomic nervous system disorders get better when an underlying disease is treated.





